Hypoglycemia, or low blood sugar, is a constant risk for those who have Type 1 diabetes. Injecting a hormone called glucagon is the mainstay of care for life-threatening situations caused by extremely low glucose levels.
MIT engineers have created an implantable reservoir that can stay beneath the skin and be set to release glucagon when blood sugar levels fall too low as an emergency backup in situations where patients might not be aware that their blood sugar is dangerously low.
This approach could also help in cases where hypoglycemia occurs during sleep, or for diabetic children who are unable to administer injections on their own, reports MIT.
“This is a small, emergency-event device that can be placed under the skin, where it is ready to act if the patient’s blood sugar drops too low,” says Daniel Anderson, a professor in MIT’s Department of Chemical Engineering, a member of MIT’s Koch Institute for Integrative Cancer Research and Institute for Medical Engineering and Science (IMES), and the senior author of the study. “Our goal was to build a device that is always ready to protect patients from low blood sugar. We think this can also help relieve the fear of hypoglycemia that many patients, and their parents, suffer from.”
Related Breakthrough in Continuous Glucose Monitoring
The researchers demonstrated that epinephrine, a medication used to treat heart attacks and prevent severe allergic reactions, including anaphylactic shock, could also be administered in an emergency using this device.
The study, which was published in Nature Biomedical Engineering, was led by Siddharth Krishnan, a former research scientist at MIT who is currently an assistant professor of electrical engineering at Stanford University.
To assist their bodies absorb sugar and keep their blood sugar levels from rising too high, the majority of patients with type 1 diabetes receive insulin injections every day. But if their blood sugar levels go too low, they develop hypoglycemia, which can cause seizures and confusion and, if left untreated, can be lethal.
Some patients carry preloaded glucagon syringes, which stimulate the liver to release glucose into the bloodstream, to help fight hypoglycemia. People, particularly kids, don't always recognize when they are getting hypoglycemia, though.
To make it easier to counteract hypoglycemia, the MIT team set out to design an emergency device that could be triggered either by the person using it, or automatically by a sensor.
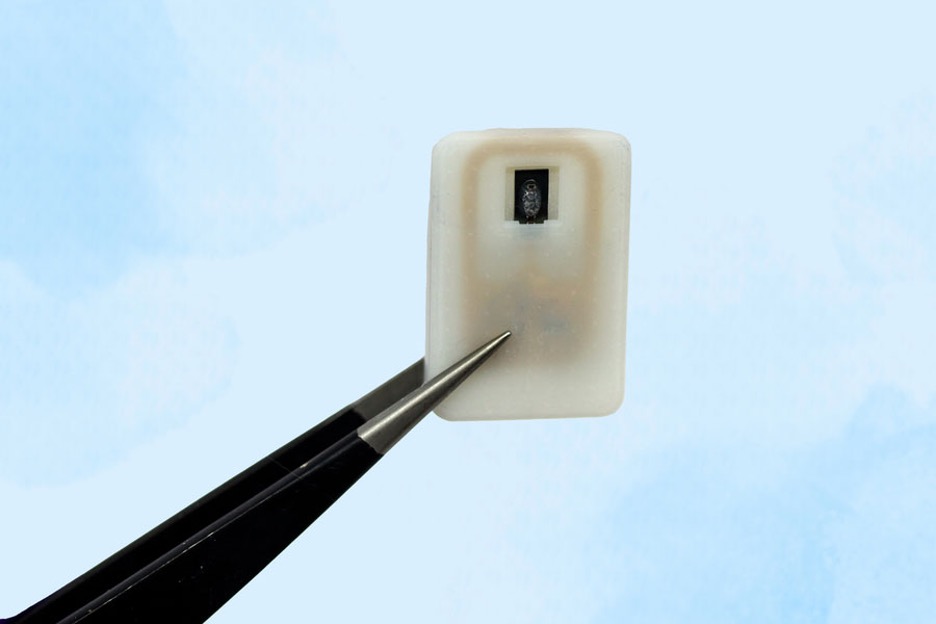
The device, which is about the size of a quarter, contains a small drug reservoir made of a 3D-printed polymer. The reservoir is sealed with a special material known as a shape-memory alloy, which can be programmed to change its shape when heated. In this case, the researcher used a nickel-titanium alloy that is programmed to curl from a flat slab into a U-shape when heated to 40 degrees Celsius.
Each device can carry either one or four doses of glucagon, and it also includes an antenna tuned to respond to a specific frequency in the radiofrequency range. That allows it to be remotely triggered to turn on a small electrical current, which is used to heat the shape-memory alloy. When the temperature reaches the 40-degree threshold, the slab bends into a U shape, releasing the contents of the reservoir.
Because the device can receive wireless signals, it could also be designed so that drug release is triggered by a glucose monitor when the wearer’s blood sugar drops below a certain level.
After implanting the device in diabetic mice, the researchers used it to trigger glucagon release as the animals’ blood sugar levels were dropping. Within less than 10 minutes of activating the drug release, blood sugar levels began to level off, allowing them to remain within the normal range and avert hypoglycemia.
The researchers also tested the device with a powdered version of epinephrine. They found that within 10 minutes of drug release, epinephrine levels in the bloodstream became elevated and heart rate increased.
In this study, the researchers kept the devices implanted for up to four weeks, but they now plan to see if they can extend that time up to at least a year.
“The idea is you would have enough doses that can provide this therapeutic rescue event over a significant period of time. We don’t know exactly what that is — maybe a year, maybe a few years, and we’re currently working on establishing what the optimal lifetime is. But then after that, it would need to be replaced,” Krishnan says.


